Summary: This article discusses the reason why coding and billing for emergency room encounters can be so difficult – and the gaps where you may be coding incorrectly leaving revenue on the table.
A broken leg. A fractured arm. Difficulty breathing. A child who swallowed a Lego. What do all these things have in common? They’re all examples of people that can be seen in the ER.
And just like you can encounter pretty much any medical situation in the ER, so too when it comes to billing for these encounters, you have to be knowledgeable about coding a wide variety of encounter types – and all the complexities that is involved.
Coding ER encounters typically have a few charges:
- Professional E/M charge
- Facility E/M charge
- Provider’s professional charge
- Facility charge such as material, supplies, equipment, syringes, band aids, etc.
While patients are physically in the hospital when they’re being seen in the emergency room, they’re not admitted – so all these charges are outpatient charges.
Plus, the ER is open 24/7 – patients are being seen around the clock and you have charges that need to be coded around the clock. It’s not the same as other services that can be coded in a typical workday.
As well, the hustle and bustle of the ED means that it’s easy for documentation to be incomplete or missing information.
This, combined with the fact that you need to code for so many different types of services, makes ED coding very complex.
Complex Coding in the ER
There are a few factors that impact the complexity of ER coding:
E/M Charges
When it comes to E/M charges, many hospitals will have some sort of automated charge capture or computer assisted software to determine the level of the professional E/M charge.
But regarding facility E/M charges, the rules are not as specific about which level to charge. For Medicare or Medicaid, they will only pay one payment.
Private carriers may still pay different fees for different visit levels. But the details of what entails different visit levels are determined by the organization itself. They must have rules established articulating what they charge for different visit levels (for example, a patient is in a room for 20 minutes, had X procedure = this type of visit level). Due to the complexity and administrative nature of this, many organizations don’t even bother to create different levels and just bill the one CMS-approved visit level, leaving revenue on the table.
The Variety of Encounters = More Complex Coding
If you have to perform a surgery in the ER, or set a fracture, or some other invasive emergency procedure – this requires more nuanced, complex coding that has to be documented properly and accounted for.
Your coders need to be:
- Specialized in coding for ED services
- Have a good general knowledge of all types of coding
- Easily understand documentation notes and pull codes from that
Infusion and Injection Charges in the ED
Missing Revenue
Finally, the most complex part of coding an ED encounter is the infusion and injection charge.
Consider:
- It’s estimated that 30% of all ED visits have a hydration infusion. But in the ED, if there is a missing stop time in the documentation, you can’t bill for that visit at all.
- If you’re missing documentation for therapeutic drugs (such as antibiotics that are routinely administered in the ED), you can only bill it as a push, and collect half
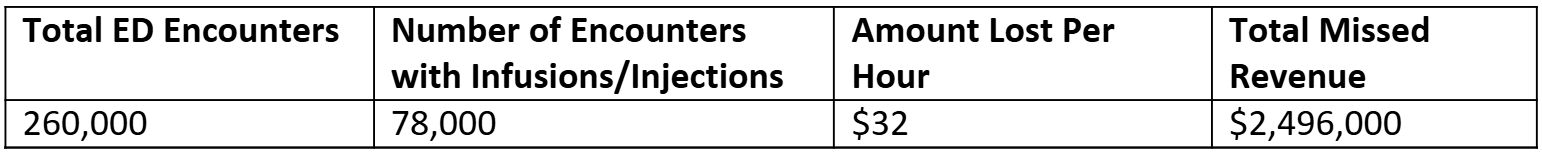
That means that imagine if you have 260,000 ED encounters, about 78,000 a year have some sort of infusion – and if they are missing stop times, you’re losing at minimum $32/hour/infusion.
Many organizations we’ve spoken to have said they don’t bill for hydration infusions in the ED at all – which is a significant reimbursement loss.
Clinical and Admin Work
Nurses and clinical staff in the ED may be expected to record start and stop times but are not as well trained as other infusion department staff in terms of documenting things correctly. As an outpatient facility, you have to bill like an infusion therapy center – and they don’t have the training or knowledge to do so. This then makes it harder for coders, who have to pull information from incomplete documentation and code from that.
Final Notes
The complexity of ED coding and billing shouldn’t be overlooked – particularly when it comes to ED infusion and injection billing. If you’re missing out on capturing these charges, let us know and we’ll let you know how much revenue you could be leaving on the table.
FAQ
1. Why is coding for emergency room (ER) encounters so complex?
ER coding is complex because every patient encounter is unique — from trauma cases to routine visits. Coders must know how to handle a wide range of diagnoses, procedures, and documentation styles, all while managing high patient volumes and incomplete clinical notes.
2. What are the main types of charges involved in ER billing?
Typically, there are several charges associated with an ER visit:
-
Professional E/M charge – for the provider’s evaluation and management.
-
Facility E/M charge – for the hospital’s use of space, staff, and equipment.
-
Professional procedure charges – for procedures done by physicians.
-
Facility charges for supplies and materials – such as medications, syringes, and bandages.
Even though care is delivered in a hospital, these are considered outpatient charges since the patient isn’t admitted.
3. What’s the difference between professional and facility E/M charges?
-
Professional E/M charges are determined by provider documentation and are often assisted by software that calculates visit levels.
-
Facility E/M charges, however, are less standardized. CMS pays one rate for Medicare/Medicaid, but private payers may reimburse different levels based on hospital-defined criteria. Many hospitals don’t create detailed visit level guidelines, which can lead to lost revenue opportunities.
4. How can missing documentation affect ER billing?
Incomplete documentation — such as missing start and stop times for infusions — can mean you can’t bill at all for certain services. For example, missing stop times in hydration infusions can cost an organization millions in lost revenue annually.
5. Why are infusion and injection charges particularly challenging?
Infusions and injections are among the most error-prone areas of ER coding. Because these depend on precise documentation (e.g., start/stop times, type of drug administered), any missing detail can lead to underbilling or non-billing.
Get the latest updates and news delivered to your inbox.
Subscribe to our newsletter today.