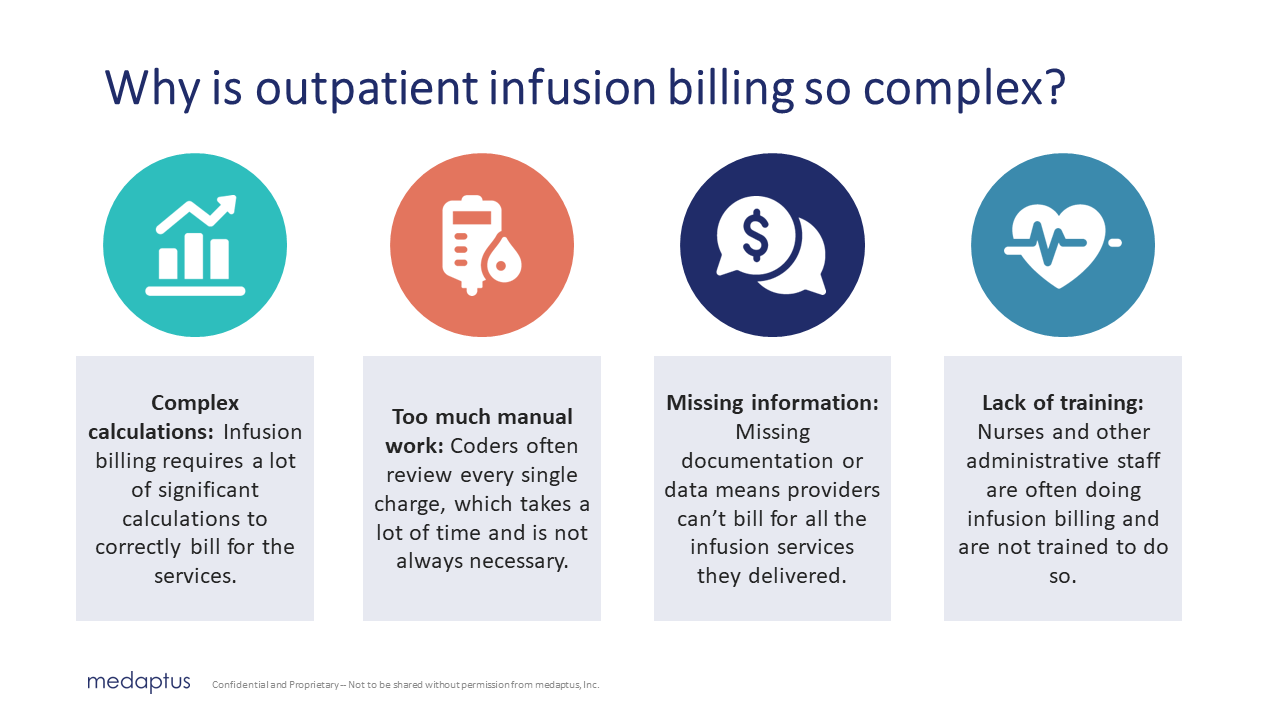
Whenever I’ve spoken to anybody that does outpatient infusion coding and billing, and I mention how complex and difficult it can be to accurately code outpatient infusion services, I get a lot of head nods, and even a few “I never want to touch infusion billing.”
Outpatient infusion billing is notoriously complex – and not something that can be done accurately manually. So what’s the difference between inpatient vs. outpatient infusion billing? And why is one more complex to code and bill than the other?
The Difference Between Inpatient and Outpatient Infusion Coding
The difference between inpatient and outpatient infusion coding is where the infusion services were delivered. This impacts what you can bill for, how you bill, and how much you can bill.
Outpatient infusion coding reimbursement refers to the reimbursement for infusion services delivered in an outpatient setting, such as a clinic, infusion center, cancer center, and it even includes emergency departments and observation clinics. Patients are typically ambulatory and are attending an “appointment” in a medical outpatient center. Outpatient reimbursement is based on a fee-for-service model, where you’re paid for each specific service – aka the infusion therapy that you deliver.
The reimbursement for outpatient infusion coding is determined primarily based on the duration of the drugs that are infused, while also considering factors such as the type of medication and the dosage of that medication.
On the other hand, inpatient infusion reimbursement refers to infusion services delivered in a hospital or other inpatient facility, for patients who have been “admitted” to the hospital. Inpatient reimbursement is usually based on a diagnosis-related group (DRG) system, where a predetermined payment is assigned to a specific diagnosis or condition. In this case, you don’t get reimbursed separately for each infusion service delivered during the inpatient stay; but rather the infusion and the other services delivered are bundled into the overall payment for the inpatient stay, based on the total DRG amount you are eligible to bill for.
Outpatient reimbursement focuses on specific services provided, while inpatient reimbursement is based on the overall care received during the inpatient stay.
One of the biggest factors that plays a significant role in outpatient infusion coding and billing are the start and stop times of delivering the infusion service. Start and stop times are typically not required in inpatient infusion coding. Here’s why.
Outpatient Infusion Coding
In outpatient settings, infusion therapy services are often coded based on the duration of the infusion – this is called “time-based coding.” The start and stop times help determine the total time the patient received the infusion. If duration of the infusion cannot be calculated due to missing start/stop times, the appropriate service billing code cannot be determined.
The start and stop times are used to calculate the number of billable units for each drug infused. Each unit typically represents a specific duration (e.g., 15 minutes), and the reimbursement is made based on these units. Longer durations require more billable units and hence, are reimbursed at a higher rate.
So accurate documentation of start and stop times ensures proper billing and reimbursement for the actual time the patient spent receiving the infusion therapy.
When start and stop times are being recorded manually, it leaves room for a lot of error – and missing revenue. For example, if no stop time is recorded, then the infusion must be automatically billed as a “push” (an infusion service that lasted less than 16 minutes). If this is constantly happening to infusion services you’re delivering, you’re leaving a lot of money on the table.
In another scenario, one hospital that I audited was automatically downgrading their stop times to under 16 minutes, when they could’ve – and should’ve – billed it as a “long” (over 16 minutes). This cost them three million dollars in underreported infusion services.
Inpatient Infusion Coding
In inpatient settings, infusion therapy services are bundled into a Diagnosis-Related Group (DRG) payment system. The reimbursement for inpatient care is based on the patient’s overall stay, including all services and treatments received. Organizations are reimbursed with one “lump sum” payment regardless of any individual services provided.
Inpatient infusion coding primarily centers around capturing the patient’s diagnosis, condition, and treatment details, rather than the specific start and stop times of individual procedures.
Since the reimbursement for inpatient care is not based on time units, the start and stop times are not as important for coding and billing purposes in the context of inpatient infusion therapy. Proper documentation is still required and may include start and stop times, but that information is not necessary to code and bill appropriately.
Final Notes
While you always want to accurately record every aspect of the services you deliver to a patient, it’s even more important to do so when it comes to outpatient infusion billing and coding. In the outpatient scenario, the start and stop times are vital to getting properly reimbursed for the therapies you delivered. If you’re not recording stop times; or if a nurse needs to write it down manually; or it doesn’t match exactly what’s in the EHR, you can be leaving thousands or millions on the table in infusion services.
That’s why we developed Charge Infusion – an automated infusion coding solution for outpatient infusion therapies. It automatically pulls the data from your EHR, removing the manual work involved, creates the appropriate charges, so you are maximizing what you can bill for – and sends it straight to billing. You can rest assured no one has to do complex calculations manually and you know you’re not missing out on infusion revenue. Learn more about Charge Infusion here.
Get the latest updates and news delivered to your inbox.
Subscribe to our newsletter today.