There have been significant changes to Evaluation and Management charges in 2023. Yet, there are still some providers that may not be fully aware of these E&M changes or what they mean for submitting charges and reimbursements. These changes have huge revenue implications for your organization.
I recently gave a talk at the medaptus Academy, a virtual user conference for our Charge Pro customers, about these changes and what they mean. Here’s a recap of what I shared.
Big Picture Changes
In documentation and billing, there have been some significant changes to requirements for documentation, specifically what the charges are going to require. These changes consist of:
- No observation codes anymore – You will just be using inpatient codes regardless of inpatient or outpatient status.
- No more counting bullet points from medical history or a physical exam. The main driver for your notes is based on the medical decision making you will be making or strictly the time that you document.
All E&M services are based on either:
- Medical Decision Making
- Time
Factors for Medical Decision Making
Medical decision making can be straightforward, low, moderate, or high. To qualify, you must meet 2/3 criteria for each category.
Up until now, time has been only used for critical care (pure time-based code) or discharge services which is also a time-based code. Now, you can use time for any codes you’re doing and can include time before, after or during the visit. This is new because now you can include things you typically wouldn’t have been able to before such as:
- Preparing for the visit
- Reviewing results
- Counseling/education of patient/family
- Ordering medications, tests, or procedures
- Communicating with other providers
- Documenting in the record
- Care coordination
- Interpreting tests
If you’re going for time-based billing, you must document all the time spent doing all these things and sum it up into one time frame.
History and Physicals – Hospitals
Most patients being admitted to a hospital under this new system should be categorized as level three H&Ps.
A level three H&P on a patient being admitted must consist of the following:
- High level of MDM (medical decision making).
- Requires two of three high level of Problems, Data, or Risk
- Problem: One chronic problem with severe exacerbation or one acute problem with threat to life or body function.
- Data: Three data points ordered/reviewed (external notes, each test, discussion with other providers).
- Risk: The decision to hospitalize is a high-level risk.
- Most patients admitted to the hospital will have at least one acute problem and need a decision on hospitalization.
If you want to do time-based documentation, it will need to be 75 minutes to quality for level 3 H&P.
What do level two subsequent visits look like?
A level two is a visit that requires a moderate level of medical decision making. Most patients should be level two. Few should be level one.
- It requires two of three moderate level of Problems, Data, or Risk
- One chronic problem with exacerbation or two stable chronic problems, or one new problem, or one acute problem with systemic symptoms.
- Three data points ordered/reviewed (external notes, each test, discussion with other providers).
- Risk: Prescription medications, limitations caused by social determinants of health, or decisions regarding surgery.
If doing the time-based model, the time spent must equal 35 minutes.
What do level three subsequent visits look like?
- A level three requires two of three high level of Problems, Data, or Risk
- One chronic problem with severe exacerbation or one acute problem with threat to life or bodily function.
- Three data points ordered/reviewed (external notes, each test, discussion with other providers.
- Medications that require drug monitoring, IV controlled substances, decision of DNR, seizure medication or de-escalating care, decisions on major/emergency surgery. Many won’t meet this criterion, but some will.
Or if time based, will need to be 50 minutes.
There are probably more level three progress notes in your practice than you realize, and you could be missing out on revenue.
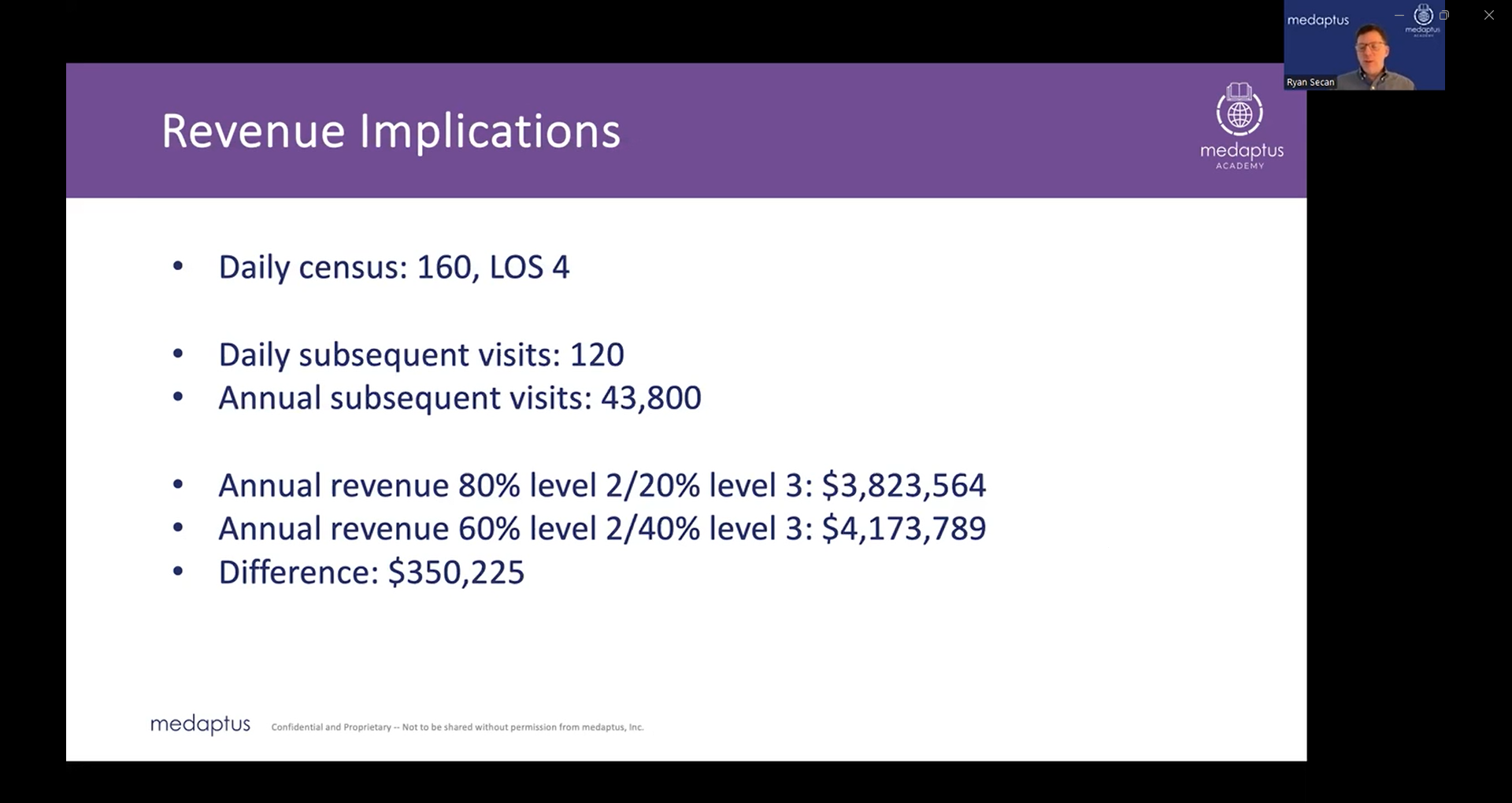
Revenue Implications
As seen below, there can be a huge difference in revenue if you are consistently billing level 2s when it could be classified as a level 3. In this example, instead of billing only 20% of visits as level two, this provider started to look at their charges and started to bill more accurately at 40% as a level three instead. The result? More than a quarter of a million dollars in revenue.
 How can you make sure you are billing correctly and maximizing revenue?
How can you make sure you are billing correctly and maximizing revenue?
- Talk to your providers about the changes in new coding rules and the importance of these changes and accurate coding.
- Demonstrate the simplicity of the new coding rules.
- Audit a sample of charts from all providers for coding accuracy.
All these things will allow your providers to focus more on providing robust documentation of history and medical decision making. What you will find is an increase in productivity, less frustration with documentation with systems that don’t matter, and will be able to focus more on medical decision making which will result in YOU capturing the revenue you need.
How Medaptus can help you:
Charge Pro’s E&M distribution reports for both the group and individual providers can help identify outliers in your charges for further chart review and use this to educate providers. You can also track changes over time in the application – you can see if you’re getting a short-term return in terms of people increasing their coding over time and maintaining a certain level of coding and ensuring they’re following compliance rules. Lastly, you can have the data you need to show administration how the hospitalist team is supporting the hospitals’ mission by creating a project that has identified coding issues, provided education, and successful increase in revenue.
Read our case study on Cox Health and how medaptus transformed their billing process from a 3–4-day charge lag to currently being able to submit charges in the same day.
Get the latest updates and news delivered to your inbox.
Subscribe to our newsletter today.