Today more than 200,000 certified medical coders work to support the documentation and billing needs of provider organizations large and small. Until widespread adoption of EHRs happened, these professionals relied on thick codebooks and training courses. Thankfully today’s advanced clinical systems usually have some degree of coding capability to lessen the onus on coders, but errors still happen given the complexity of coding rules and frequency of changes. Regardless of the reason why, when these errors are committed, groups experience denials, rework, reduced revenue, and possibly even provider ire.
So, what are common coding errors that might be easier to fix than you think? And what is the data needed to fix habitual errors that could be costing medical groups money?
E&M Outliers
Coding for evaluation and management services (E&M) should resemble a bell curve with most patients needing average levels of care, with outliers on both ends of the spectrum. Running a simple analysis on the distribution of E&M level codes by category at least monthly gives the opportunity to identify patterns that may represent a lack of coding knowledge. Or perhaps these insights point to a provider caring for sicker patients who may be feeling overworked. In the event of coding ignorance, familiarizing newer providers with the AMA’s criteria for E&M levels is a smart place to start.
Medical Billing Statement
Habitual Errors
When it comes to coding rules, the type and number of rules that govern reimbursement is dizzying. CCIs, LCDs, NCDs, Medicare rules… the list goes on. Understanding if one class of rules is causing more downstream work could point to a process failure. For example, local coverage determination rules are updated quarterly so if there are higher than expected LCD issues, has your billing vendor updated its dataset?
Near-time Provider Feedback
Providers are naturally curious people. While they will never have deep understandings of medical coding, they do have “skin in the game” and are open to feedback especially when it comes to billing and payment. If a coding team recognizes that a provider is overlooking a coding opportunity or coding something incorrectly, getting that feedback to the provider in a timely manner is much more impactful than reviewing at a staff meeting weeks later. Embedded messaging is immensely helpful to foster this communication.
Point of Care Compliance Enablement
Moving coding intelligence as close to the point of care as possible means removing error from the middle of the revenue cycle. Though it may be tempting to trigger real-time alerts directly to providers around possible coding errors, there is risk of contributing to overall alarm fatigue. While documentation or code selection by a provider may be linked to errors, if the provider doesn’t have the knowledge to quickly correct the problem, this should be reviewed in a coder work queue. Applying proactive coding rules to provider workflows must make sense in terms of the timing and providers must be empowered or educated to address the alert in order for it to be helpful.
Pro Forma Mini Audits
Instead of waiting for an issue to grow in size and be uncovered by an audit or records review, start undertaking mini audits related to specific encounter types, from multi-procedure to specific payer. Use any learnings to adjust workflows, training aids, or even software configuration depending on results. Take this a step further and calculate the estimated impact of potentially identified issues in order to connect the dots as to why correct coding is so critical.
Though certified coders are exceptional at supporting clinical documentation and billing workflows, educating physicians with appropriate pieces of actionable information can reduce re-work and increase productivity. Collaboration backed by an effective toolkit can drive productivity and bottom-line efforts without significant investment or time overhead.
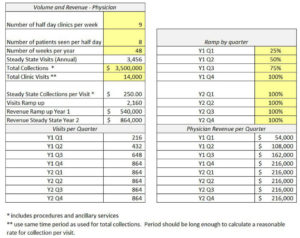
Pro Forma Financial Statement Example
Get the latest updates and news delivered to your inbox.
Subscribe to our newsletter today.