The hospital medicine specialty is only about 20 years old but today has over 50,000 providers including MDs and DOs along with advanced practice providers. This relatively small group found itself at the center of America’s COVID pandemic response in 2020. Countless hospitalists worked tirelessly to save lives in overburdened units while quarantining from loved ones and confronting helplessness as patients were dying alone in isolation.
While the COVID situation is now steadily improving here in the United States, hospitalist groups have emerged battered and now face new challenges. Physician burnout is rampant and for many groups, finances are concerning. Hospital medicine providers have never worked harder days or longer hours, but their efforts could not financially offset the lack of procedural and elective revenue for most healthcare systems.
To help hospitalist groups recover financially, charge capture technology remains an essential tool in their revenue cycle toolkit. With functionality built specifically for hospital medicine groups and the unique characteristics of hospital admissions, today’s charge capture solutions are effective in preventing lost service revenue.
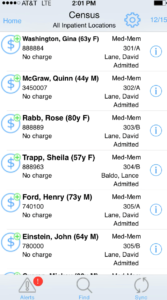
Hospitalist Rounding List
Key capabilities within a robust, hospitalist-centric charge capture platform that are demonstrated to drive overall revenue capture and associated operational efficiencies include:
Electronic rounding lists are effective in generating personalized lists for providers either as individuals, or as a team. If support personnel in the coding department lack visibility into these lists, ensuring complete charge capture over a multi-day is a challenge, especially when multiple providers were involved. Technology that ties the presence of a patient on a list to a charge opportunity, and with coder-centric reconciliation tools to identify missing charges, eliminates lost revenue.
With hospitalists being on the front lines of medicine and treating illness across a number of clinical areas, the potential to be impacted by annual code set changes and payer rule updates is high. Savvy revenue cycle teams take the learnings from payer denials to prevent future denials for the same reason. Charge capture platforms with custom rules engines can ensure that charges meeting criteria are flagged for review pre-billing to prevent the cost of a denial re-work.
Streamlined Back Office Throughput
For revenue teams looking to improve KPI performance, throughput is a good place to start. How many patient charges can a team process per day? What if the practice wanted to grow – how can a hospitalist team scale without tipping the FTE scales? Exception-based workflows are a proven way to increase efficiencies. Using charge capture technology to drive fast and accurate charge capture, with review and reconciliation tools enabling the automatic identification and billing of “clean” charges, can increase throughput by fifty percent or more. Only charges flagged for possible errors require review while the rest are sent to billing automatically.
Charge to Documentation Reconciliation
Earlier this piece reflected on the importance of reconciling missing charge activity to rounding list data in order to ensure 100% of charge opportunities have been capitalized on. Another similar feature that hospital teams enjoy is the ability to reconcile E&M visits with the presence of clinical documentation. Charges lacking submitted documentation can hold until the note is in, again saving time with follow-up activities and ensuring the provider has selected the appropriate level of care.
Identifying Relevant Trends and Patterns
Charge capture platforms typically offer reporting tools to share insight around gaps, existing bottlenecks, and patterns. Sharing such reporting with providers to change behavior can be effective at preventing ongoing and habitual coding or documentation errors. Trending data can also be used to review overall group performance to identify opportunities for improvement in quality and lag to further shore up revenue cycle performance.
Curious to learn more about medaptus’ revenue cycle management offerings for hospitalist medicine teams? Reach out to us here.
Get the latest updates and news delivered to your inbox.
Subscribe to our newsletter today.